Local Practice
Long-term sustainability through place-based health
Author: Zayn Qureshi |

Although its principles are now well-established and practiced, the full promise of a total place approach to area budgeting and comprehensive public service reformation in localities remains unrealised. At a time when ministers and officials are straining all means necessary to funnel billions of pounds from the health service’s 70th anniversary budget boost into shovel-ready NHS schemes, there is a moral case for making population health and place investment count for the fullest amount possible.
Local Practice is a case for place that is centred not around the need for power transfer, but a localist case to liberate resources, assets and latent potential that exist within every community. It is a call to rationally manage limited resources and deploy data and new technology for the best results. It is a simple prescription to integrate agents of health and guardians of place at an appropriate level for the sake of delivering human-centred care to local populations through all stages of life.
Download the Executive Summary
Download the Recommendations
Download the annexe: Major challenges confronting the NHS today and what reforms are needed to provide long-term sustainability in a challenging funding environment by Dr Geoffrey Boxer and Linda Boxer
Key Points
Local Government & Public Health
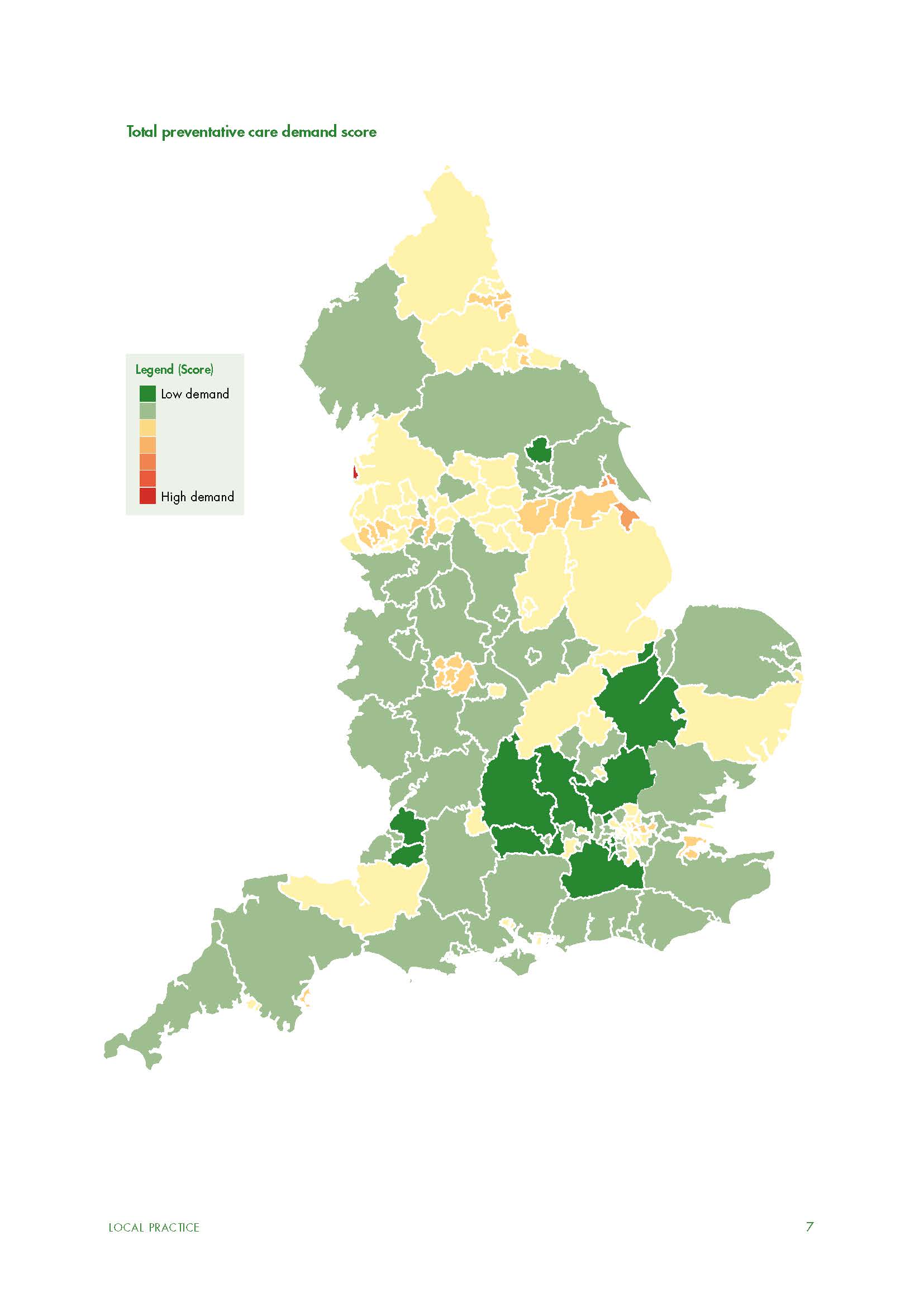
There is a symbiotic unity between our life and our environment. Inhabitants from the least deprived areas of England on average live for twenty years longer than those in the most deprived. The health of a community is therefore inseparable from place and prosperity. Furthermore, the prosperity of place aggregates up to the benefit of the national economy. Given the renewed focus on prevention, it is only natural that local authorities be leaders in the fight against public health challenges and how they manifest in communities. Local authorities with a public health duty be provided with a Prevention Premium, modelled after the Pupil Premium grant for school funding, to help support the transition to public health delivery interlinked across all council functions and wider civil society actors and institutions.
The Role of Place in the NHS
The other side to the coin of the local authority role in public health is the self-responsibility of individuals to look after their own health. Government needs to become more serious about developing and encouraging consumer-led healthcare, focusing on methods for disease prevention and reducing demand by incentivising individuals to look after their own health better. It would be nice to think that the delivery of healthcare can always be a simple and smooth process, but reality is very different and perhaps we should start to think of how we react to symptoms of serious disease more like we do for accident and emergency. Since its inception the NHS has failed dramatically to understand the full value of all the data that it generates and holds, and the information and knowledge that this yields. The sharing of NHS patient data will continue to be viewed with more than a little suspicion by the general public with regards its security and anonymity – especially once stored in data warehouses that are external to the NHS. If patient data is to be used across silos to improve care, it is of paramount importance to deal with the fears and trust of the general public.
Staffing the NHS and Social Care
Compounding the myriad issues facing the health economy discussed throughout this report is the worrying level of workforce vacancies it now routinely faces. Heath and social care has always relied, to varying degrees, on immigration to fill staff shortages. Migrants make a unique contribution to the sector and are doing more than simply substituting for British labour; they are filling skills gaps the British working age population seem unwilling to plug. Ongoing Brexit uncertainty has had an impact on the health and social care sector as more potential care workers are deterred from entering the UK jobs market. Migration policy should not intensify the problem by placing obstacles in the way of recruiting the skills and labour the sector needs. This involves a necessary boost of investment into the social care budget, which would allow for raising wages, and creating new opportunities and prospects for social workers. A comprehensive immigration system that puts place-based needs first is essential post-Brexit
